When It’s More Than Just “Getting Older”
It can start subtly. A loved one begins shuffling their feet, forgetting appointments, or making more frequent trips to the bathroom. Often, these changes are dismissed as part of aging. But what if it’s more than that? Normal pressure hydrocephalus (NPH) affects approximately 5% of adults over 65 and is one of the few neurological conditions that is not only treatable, but potentially reversible. And yet, up to 80% of cases go undiagnosed.
The key to changing that starts with recognition, and asking the right questions.
The Classic ‘Triad’ of NPH Symptoms
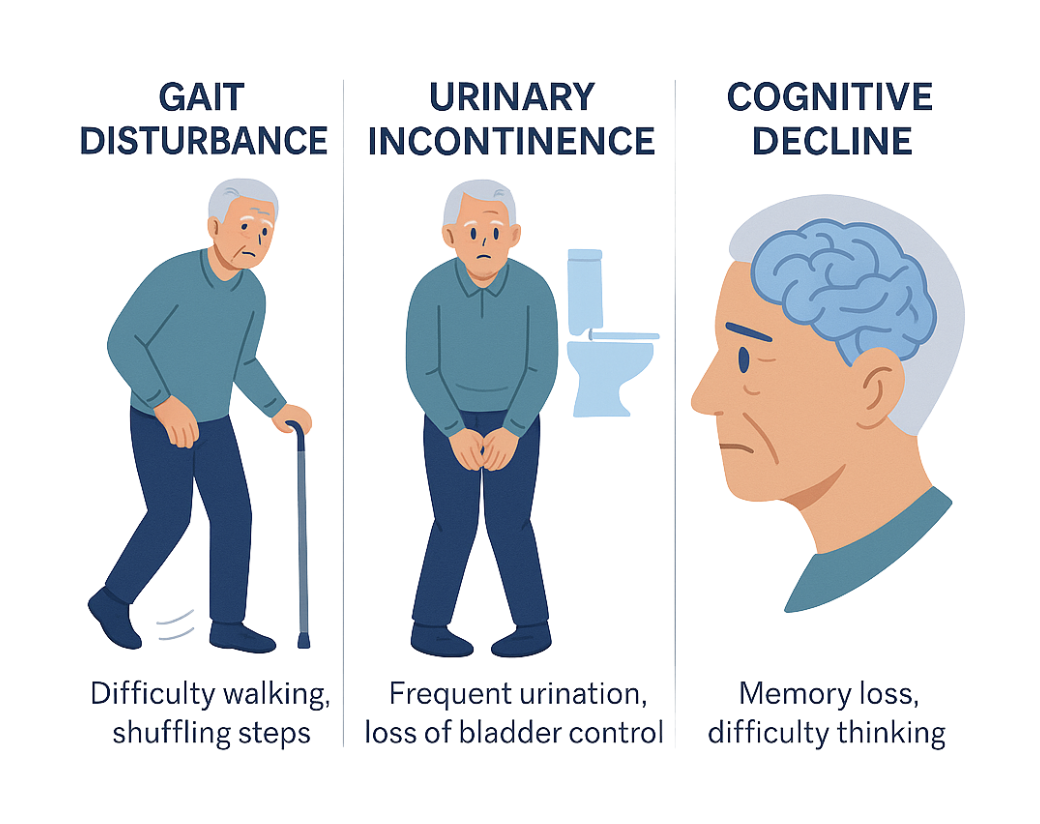
NPH presents with a distinct triad of symptoms. While each symptom on its own may be overlooked, together they form crucial diagnostic clues:
- Gait disturbances: Typically the earliest and most prominent symptom, patients often walk with short, shuffling steps. They may appear unsteady, have trouble initiating walking, or feel as if their feet are “glued” to the floor.
- Urinary incontinence: This may begin as increased urgency or frequency, eventually progressing to full incontinence. Because it’s an embarrassing symptom, it’s frequently underreported.
- Cognitive decline: Subtle at first, cognitive symptoms may include slowed thinking, reduced attention, and memory lapses. Unlike Alzheimer’s disease, this decline can often be reversed with proper treatment.
These symptoms can resemble other conditions common in aging, such as Alzheimer’s or Parkinson’s disease, contributing to the frequent misdiagnosis. Not every case of unsteadiness or forgetfulness is cause for alarm, but the combination of gait changes, urinary problems, and cognitive issues should raise red flags and prompt a request for testing.
What to Ask Your Doctor
If you suspect NPH, your doctor may recommend brain imaging such as a CT or MRI. These can reveal enlarged ventricles (ventriculomegaly), a hallmark of the condition. But imaging alone is not enough, as ventriculomegaly can also occur in other neurodegenerative diseases.
To confirm NPH, secondary, more specific tests are often required: cerebrospinal fluid (CSF) infusion testing can be one of the most effective diagnostic tools. This test assesses CSF outflow resistance (R(out)), a key indicator of how well the brain is resorbing and adapting to cerebrospinal fluid pressure. Elevated R(out) is strongly associated with NPH.
Early Detection Leads to Better Outcomes
The most hopeful part of an NPH diagnosis is this: it’s treatable. Many patients who undergo shunt surgery after proper testing experience dramatic improvement in mobility, continence, and cognition, with benefits lasting five years or more.
However, the benefits are greatest when treatment occurs early. That’s why recognizing symptoms and requesting the right diagnostics is critical.
At X-Pressure, we’re committed to improving NPH detection and reshaping the future of aging by bringing the XP One device for CSF infusion testing to the bedside – supporting clinicians in making earlier, more confident diagnoses and giving patients a real chance at recovery.
